Hiatal Hernias
Hiatal hernia (hernia stomach), is a prolapsed (herniated) parts of the stomach through the esophageal opening in the diaphragm into the chest. Hernia consists of a hernia sac formed by the peritoneum and in which the most common is a part of or the entire stomach sometimes, but rarely can find other organs such as the stomach, small and large intestine, spleen or omentum. If there is a hiatal hernia, the normal mechanics of preventing reflux of gastric contents into the esophagus is almost nonexistent, so that symptoms such as heartburn and regurgitation in these people very frequent. Hiatal hernia are present in about 50% of the population, but nearly half of them do not have any problems. Most classification implies the existence of four types of hiatal hernia: Type I or sliding (sliding, axial), type II, or paraesophageal (rolling, kontrljajuće), type III or mixed (mixta) and type IV, combined hiatal hernia. Only adequate and complete diagnosis allows the right choice of treatment of these patients.
Details on the types, causes of, symptomatology and diagnosis of hiatal hernia see below.
Introduction
Diaphragmatic hernia can be congenital, which is rare, or acquired. Acquired diaphragmatic hernia, on the other hand, can be traumatic when abstracted any region of the diaphragm or nontraumatic. Hiatal hernia, there are more than 60% of people over 50 years while the reflux esophagitis and thus gastroesophageal reflux disease (GERD) is present in 75% of patients with hiatal hernia, of which only 50% have problems.
The acquired non-traumatic hiatal hernia are classified depending on the position of the compound of the esophagus and stomach (gastroesophageal transition) and surrounding organs in relation to the diaphragm 4 main groups:
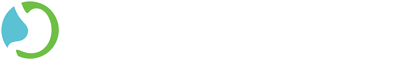
1) Type I – sliding, sliding hiatal hernia – is characterized by herniation of the proximal gastroesophageal crossing through the esophageal hiatus of the diaphragm in the posterior mediastinum (sredogrudje). The exact incidence of these hernia is not established with certainty whether the incidence somewhat more common in women with this type far the most common and makes 92% of all hiatal hernia.
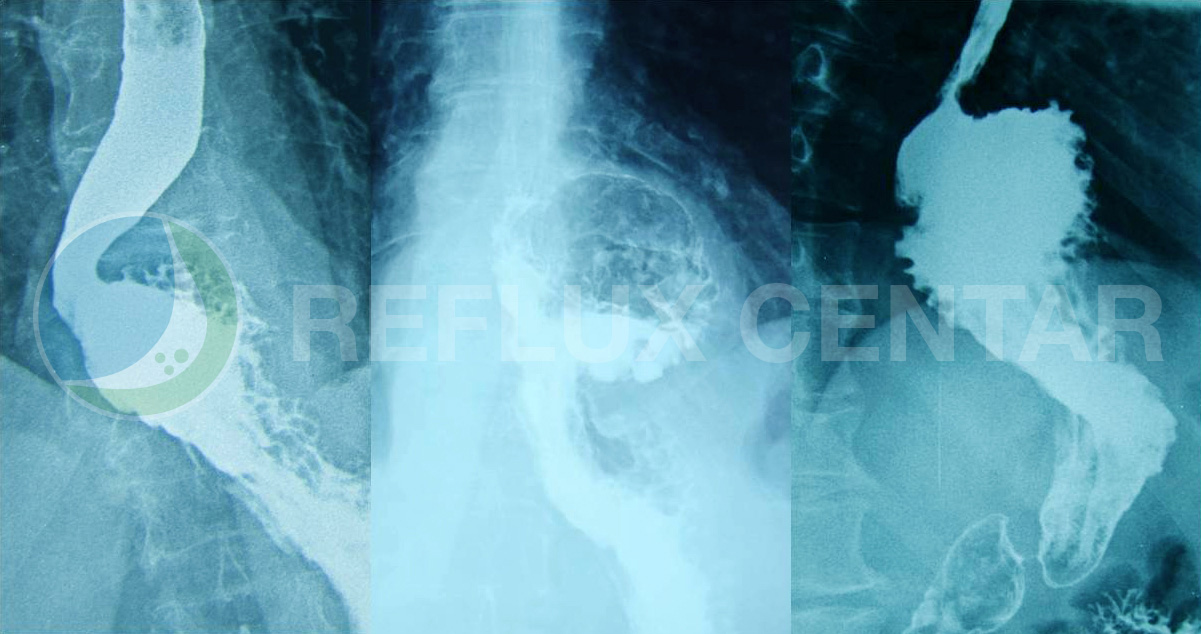
2) Type II – rolling or Paraesophageal hiatal hernia – gastroesophageal transition is in its normal anatomic position in the abdomen, but there is a herniated fundus of the stomach near the esophagus in the thorax. The frequency of true paraesophageal hernia is only about 1%, while in combination with sliding or type III and type IV consists of a total of 8% of all hiatal hernia.
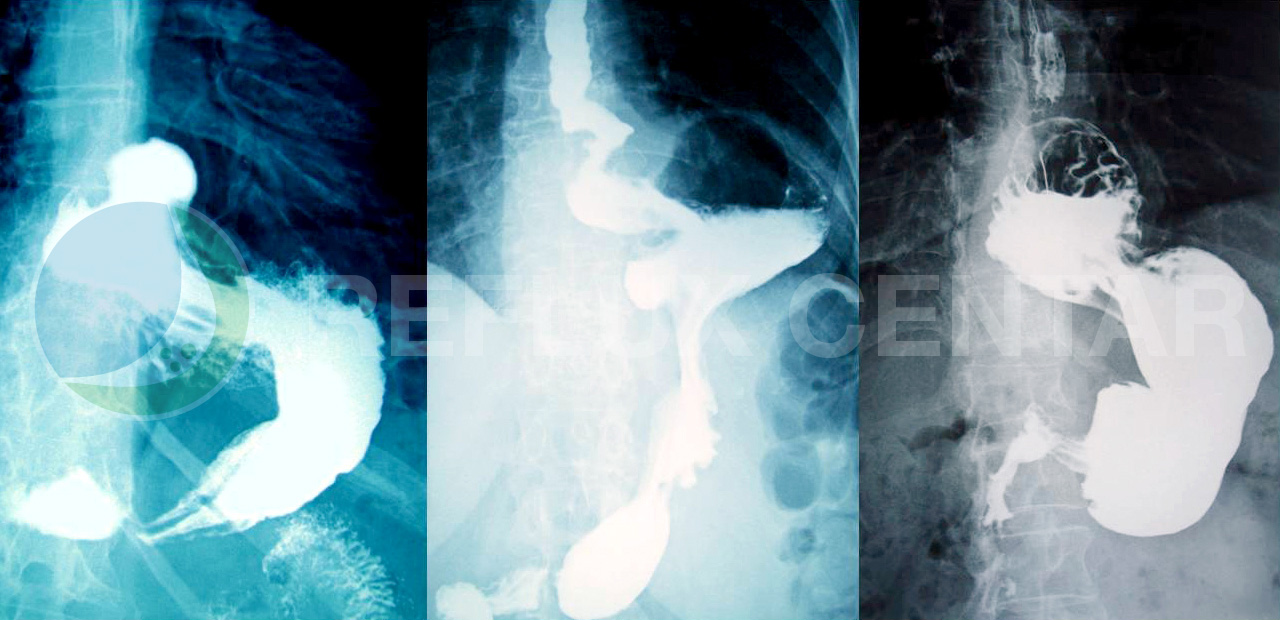
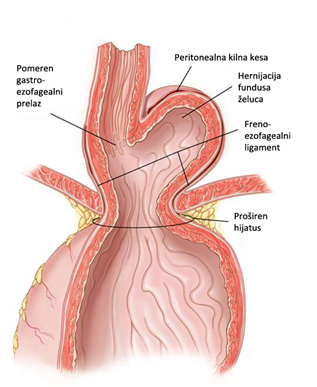
3) Type III – mixta or combined hiatal hernia – is a large hiatus hernia esophagus and is characterized by herniation combined proximal gastroesophageal transition and fundus of the stomach through the wide open esophageal hiatus in the diaphragm.
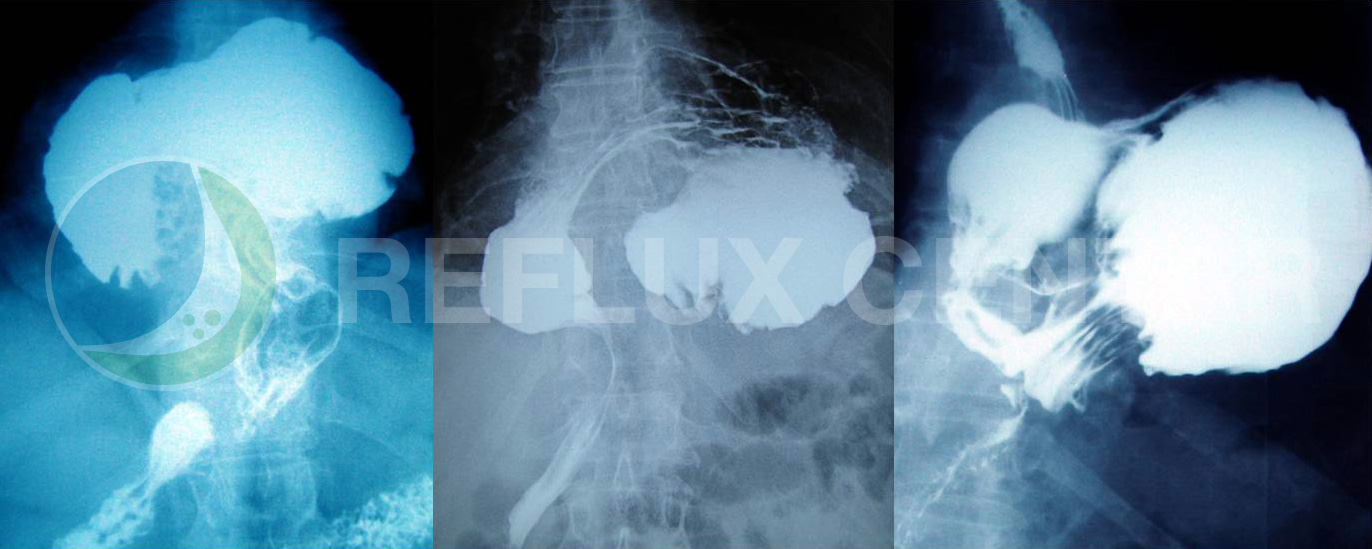
Venter reversus, upside-down stomach, intrathoracic stomach from twisting (volvulus) is the final stage of gastric hernia type I and type II or type III large hernia that occurs when the entire stomach migrates into the chest where it rotates 180 ° around its longitudinal axis with gastro-crossing and pyloric that are in fixed points. In these situations, most proximal to a large curvature of the stomach.
4) Type IV – a large defect in the diaphragm opening of the esophagus near the stomach that lets other organs such as the stomach, small and large intestine, omentum and spleen, to enter the chest. Hernia type IV represent a natural extension of type III.
| Type | Hiatal hernia | Frequency% |
|---|---|---|
| AND | Axial, sliding (sliding) | 92 |
| II | Paraesophageal (rolling) | 1 |
| III | Mixed (a combination of the first two, mixta) | 5 |
| IV | Apart from the stomach into the bag kilnoj are other abdominal organs | 3 |
Axial, sliding hiatal hernia
Given that prtisak pain greater than the pressure in the chest, is facilitated by the herniation of the stomach into the thorax. Any further increase in abdominal pressure (coughing, straining, pregnancy) further emphasizes this herniation. Due to the constant pressure difference the circuit between the esophagus, the stomach and the diaphragm over time and thus allows the upper part of the stomach to pass through an opening in the diaphragm. When told herniation, connection between the esophagus and the stomach moves up through the hiatus. If there is associated damage to the lower esophageal sphincter (DES), will develop GERD. Endoscopic studies indicate that approximately 80% of patients with GERD have an axial hiatal hernia esophageal which represents a significant difference compared to the healthy population (about 40%). It is estimated that prevalnca hiatal axial type in Europe is on average about 45%.
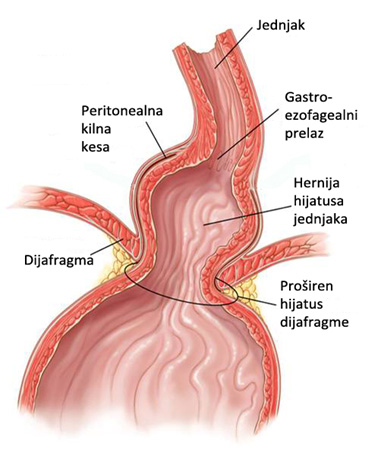
Most patients with sliding hiatal hernia have no symptoms and it is usually detected incidentally during radiographic or endoscopic examination. The diagnosis of this disease, it is important to detect the existence of the hernia and to determine whether the reflux of gastric contents causing esophagitis. The incidence of hiatus hernia increases with age so that people in the 60’s have a prevalence of about 60%. The clinical course of patients with this kind of herniation has no more importance or consecutive occurrence (approximately 85% of patients), reflux esophagitis is a particular problem.
The exact reason for the emergence of sliding type of hiatal hernia is not yet known, but is thought to be most likely due to a combination of several factors which include primarily a disorder of connective tissue with consequent muscle weakness and chord part of diaphragm, as well as increased pressure in the abdomen.
A more detailed classification of axial hiatal hernia is based on progressive stages of moving the EEA in the chest. This classification describes the stages depending on the total shortening of the esophagus, and is divided into three basic forms:
1. failure hiatus
2. concentric hiatus hernia esophagus
3. Quick esophagus.
The boundary between the first and second group represents the displacement of more than two centimeters of the stomach to the chest. Unlike insufficiency hiatus where radiographic does not verify the existence of hiatal hernia, but proving endoscopy, radiographic verification is evident in the concentric type. The basis of the division of sliding hiatal hernia the smaller and larger than 2 cm is located in the functionalities of DES. It has been shown that patients with GERD, but without a hiatus hernia or hiatal hernia with less than 2 cm have almost identical basal pressure, total and intra-abdominal length DES. On the other hand, in patients with GERD and hiatal hernia greater than 2 cm there is a significant reduction of all three parameters (basal pressure, total and abdominal length DES), which represent the backbone of antirefluskne barriers and functionality of the DES.
In some cases, patients with hiatal sliding type and chronic GERD, and comes to the appearance of peptic narrowing (stenosis). In the initial stages of this disease is caused by narrowing of the esophagus edema and muscle spasm and is reversible phase. Frequent reflux leads to a circular progressive tissue damage extending through the wall of the esophagus. The final result of this process occurs scarring that leads to the formation of a typical scar tissue with consequent irreversible narrowing. Thus affected segment of the distal esophagus, mainly thickened and shortened, primarily due to the contraction of scar tissue. The prevalence of peptic stenosis in patients with GERD is on average about 10%, and the process of narrowing begins to skvamocilindričnom crossing and generally is 1 cm long, but can be much longer.
Paraesophageal hiatal hernia
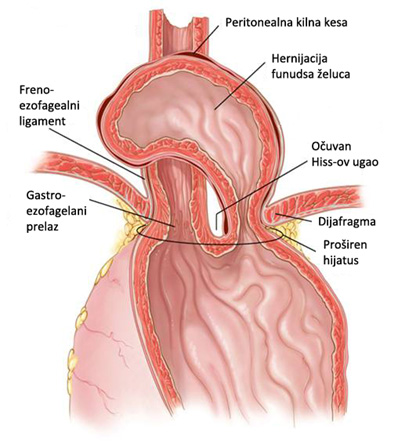
In patients with type II or paraesophageal hiatal hernia there is a defect in the diaphragm on the left side of the esophagus, or extreme weakness of the so-called. Kruse left hijatalnog opening. With this type of hernia, cardia of the stomach or EEA remain positioned in the abdomen, while only fundus of the stomach protrude through the defect dijafragamalni beside the esophagus. The natural history of this type of hernia is progressively increasing, which leads to the appearance of the first mixed-type hernia, and in its final phase and twisting of the stomach (volvulus) where there is a convergence pylorus and cardia of the stomach, and to give the complete positioning of the stomach in the chest. In these patients, the most common symptom is dysphagia, heartburn and not due to pressure from the upper part of the stomach to the last part of the esophagus. These types of hernias are extremely rare in daily clinical practice. Row subgroup paraesophageal hernia represent patients with “parahijatalnim hernia” under which the preservation of individual muscle fibers of the diaphragm between the esophagus and gastric fundus.
Mixed and combined hiatal hernia
In patients with type III or mixed hiatal hernia leads to a significant weakening and stretching the opening of the esophagus to the diaphragm, causing a combined displacement EEA and fundus of the stomach to the chest.Most likely, this type of hernia primarily began as type II, but was due to strength and progressive enlargement of the esophagus openings, primarily his left, comes to moving the EEA above the diaphragm.While the right type II paraesophageal hiatal in clinical practice very rarely seen, Type III is much more common.Patients with this type of hernia are in addition to the feeling of heartburn and very frequent regurgitation accompanied by frequent coughing due to the reflux of gastric contents into the tracheobronchial tree.
Combined Type IV hiatal hernia esophagus are associated with the greatest defect in the opening of the diaphragm, whereby in addition to the stomach leads to the herniation of other intra-abdominal organs: the great omentum, spleen, small intestine and colon, the left lobe of the liver and sometimes the pancreas.These types of hernia is called “upside down stomach” or venter reversus, since they are usually accompanied by a complete positioning of the stomach in the chest, with subsequent twisting of the stomach (volvulus) around its vertical or horizontal axis.In some cases, patients with this type of hernia and gastric volvulus may have triad of symptoms which was first described by a German surgeon Moritz Borchardt (1868 – 1948): severe pain in the epigastric or behind the breastbone, burping strongly but without vomiting and inability to qualify nasogastric tube.Most doctors this group is considered an advanced phase of the mixed hernia, so it’s generally not singled out as a separate entity.
Symptomatology of patients with large hiatal hernia is often very nonspecific and can point to some diseases completely different organs.People with large hiatal as the primary symptom may have a dull pain in the ribs or in the very Gudima, shortness of breath (due to pressure from itself žludačne hernia diaphragm) and heart palpitations (mainly due nadržaja the vagus nerve, as well as directly to the heart muscle and large blood vessels).Very common symptoms of these hijatalnih hernia also include early satiety and chest pain after eating and regurgitation generally poorly digested food.Symptoms of heartburn are rarer in these patients, because a large stomach hernia pressure final part of the esophagus and thus partially prevents the stomach acid.
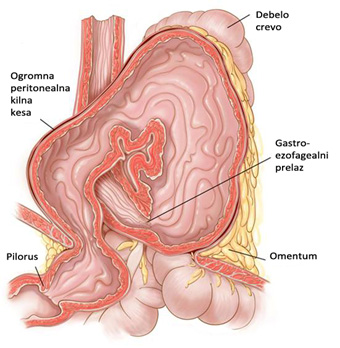
Complications of the existence of Type II, III and IV hiatal hernia, are mainly mechanical nature:
1) ulcers, the level where the diaphragm exerts pressure on the stomach and consequently prevents adequate circulation, with consequent hemorrhage, necrosis and eventual perforation (Cameron’s ulcers)
2) dysphagia or afagija, due to the pressure in the gastric fundus to the last part of the esophagus due to complete or twisting of the stomach in the chest
3) extraesophageal, laringotraheopulmonalne, manifestations usually due to aspiration of gastric contents into the bronchial tree and lungs.
Diseases
- Anatomy and Physiology of the Foregut
- Gastroesophageal Reflux Disease (GERD)
- Barrett’s Esophagus
- Hiatal Hernias
- Achalasia
- Esophageal Motility Disorders
- Esophageal Diverticula
- Helicobacter pylori gastritis
- Peptic Ulcer Disease (PUD)
- Gallstones (Cholelithiasis)
Lexicon
Patients Informations
Soon
If you have more questions contact us:
info@refluxcentar.com

 српски
српски